Do you often feel like your heart is beating out of control or that your chest is heavy? If so, you must know that these are only a handful of the frightening indicators of a cardiac emergency. Heart disease still remains to be the primary cause of death across the world, taking millions of lives annually. Millions of cases of sudden cardiac arrest (SCA) are reported each year, making it one of the most prevalent and dangerous emergencies. The frequency of cardiac emergencies reflected substantial variation, with an average of 62 instances per 100,000 individuals and a range of 35.7 to 128.3 cases. Additionally, there were differences in survival rates, ranging from 1.6% to 20.7% according to NCBI study.
It's interesting to note that populations with high rates of incidents usually had lower survival rates, meaning that as the number of cases increased, the survival chances decreased. It is imperative that symptoms such as dyspnea, abrupt exhaustion, or erratic heartbeat be promptly identified. Not only is prompt response essential in these dire situations, it can save lives. The first line of defence against an invisible threat for you and your loved ones is knowing what to look out for and how to react.
In this blog, we will integrate the improved understanding of cardiac emergencies so that you stay informed and prepared vital for both prevention and emergency response.
What Are Cardiac Emergencies?
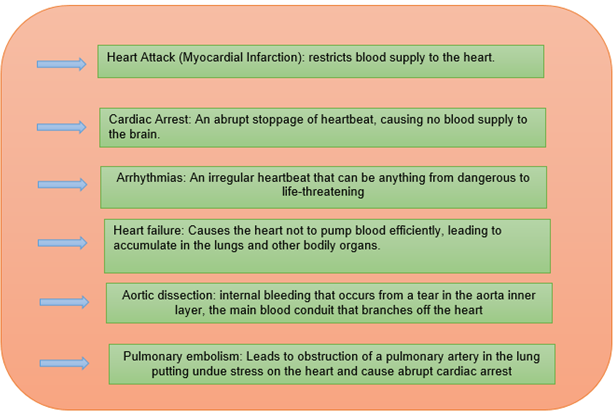
Any circumstance in which the heart's ability to pump blood is impaired and could potentially be fatal if left untreated is referred to as a cardiac emergency. A variety of conditions, including heart attacks (myocardial infarction), cardiac arrest, arrhythmias, and heart failure, are included in this category of emergencies. For each of these disorders to stabilise the patient and stop additional damage to the heart and other essential organs, specific therapies are needed. These conditions also present different problems.
What Are the Types of Cardiac Emergencies?
Different forms of cardiac emergencies exist, each with unique origins, symptoms, and treatment modalities:
What Are the Symptoms of Cardiac Emergencies?
It's critical to identify the symptoms of cardiac emergencies to receive treatment quickly. While each ailment will have its own unique set of symptoms, there are several common ones to watch out for:
- Chest Pain or Discomfort: This is a primary indicator of a heart attack and is frequently characterised as a squeezing, pressure, or fullness in the chest.
- Breathlessness: Breathing difficulties, especially during rest, maybe a sign of a major cardiac problem.
- Abrupt dizziness or lightheadedness: These symptoms could be signs of a major cardiac condition, such as a cardiac arrest.
- Palpitations: The sensation of powerful, fast, or irregular heartbeats may indicate an arrhythmia or other cardiac emergency.
- Nausea or vomiting: Some people, particularly women, may feel nauseous or throw up after having a heart attack
- Sweating: Excessive, unexplained sweating, sometimes referred to as cold sweat can occur in conjunction with cardiac emergencies.
- Loss of Consciousness: Sudden or fainting unconsciousness is a dangerous symptom that could be indicative of cardiac arrest.
What Are the Causes of Cardiac Emergencies?
Heart attacks can be caused by several underlying diseases and way of life choices. Among the frequent reasons are:
- Coronary Artery Disease (CAD): The most prevalent cause of heart attacks is caused by plaque buildup narrowing or obstructing the arteries supplying blood to the heart muscle.
- High blood pressure: It is often known as hypertension which can weaken the heart and blood arteries, increasing the risk of heart failure and other cardiac problems.
- Arrhythmias: A few different kinds of arrhythmias have the potential to induce cardiac arrest by causing the heart to stop beating efficiently.
- Atherosclerosis: A disorder that causes fatty substances to build up in the arteries, raising the risk of heart attacks and other cardiac problems.
- Diabetes: Cardiovascular condition, which can result in a cardiac emergency, is more common in people with diabetes.
- Smoking: Smoking destroys blood arteries in the heart and heart itself, which raises the risk of heart attacks and CAD development.
- Obesity: Carrying too much weight puts stress on the heart and raises the risk of conditions like diabetes and hypertension, which both worsen the chance of cardiac emergencies.
- Family History: An individual is more likely to experience a cardiac emergency if there is a history of heart illness or sudden cardiac death in the family.
What Are the Risks and Complications of Cardiac Emergencies?
Cardiac emergencies carry significant and frequently fatal risks and complications such as.
- Death: Cardiac arrest is lethal if treatment is delayed. If treatment for heart attacks and other cardiac emergencies is delayed, there is also a significant chance of death.
- Damage to the Heart Muscle: A heart attack has the potential to permanently harm the heart muscle, which could result in heart failure and diminished cardiac function.
- Brain Damage: Lack of oxygen during cardiac arrest can cause brain damage, particularly if resuscitation is not started right once.
- Multiple organ failure resulting from inadequate blood supply during a cardiac emergency can complicate recovery even more.
- Stroke: Blood clots that originate from heart attacks or in people with specific arrhythmias have the potential to go to the brain and cause a stroke.
- Recurring Heart Problems: People who have survived cardiac emergencies are more likely to experience further heart problems in the future, such as heart failure and recurring attacks.
How to Recognise a Cardiac Emergency?
Given how quickly cardiac emergencies can worsen, it's crucial to recognise one to receive prompt medical attention. Sudden, acute symptoms that require quick attention are frequently present in cardiac emergencies. Deep chest discomfort, trouble breathing, an abnormal or fast heartbeat, lightheadedness, dizziness , and fainting are important symptoms to be aware of.
Some people may experience pain radiating to their jaw, neck, arms, or back, which may be a sign of a heart attack. Knowing these warning signs can help you take immediate action, which could result in a lifesaving outcome. Once a cardiac emergency is suspected, medical experts will conduct a number of diagnostic tests to confirm the diagnosis and choose the appropriate course of action. Imaging, laboratory testing, and clinical assessment are frequently used to diagnose cardiac emergencies:
- Electrocardiogram(ECG): This test can identify arrhythmias, heart attacks, and other heart disorders by recording the electrical activity of the heart.
- Blood testing: These tests can help diagnose heart attacks by measuring the amounts of specific enzymes and proteins that are released when the heart muscle is injured.
- Chest X-ray: This diagnostic tool can identify fluid in the lungs, an indication of heart failure, and show the size and form of the heart.
- Echocardiogram: It is a type of cardiac ultrasonography that helps diagnose a variety of cardiac disorders by providing precise images of the anatomy and function of the heart.
- Cardiac MRI: A thorough imaging examination that can be used to diagnose complex cardiac problems, providing high-resolution images of the heart and blood arteries.
- Stress Tests: By evaluating the heart's response to physical stress, these tests help to detect underlying cardiac problems that may result in life-threatening situations.
What Are the Treatment Options for Cardiac Emergencies?
Depending on the particular disease, treatment for cardiac emergencies might vary, but frequently involves the following interventions:
- Medication: Beta-blockers, anticoagulants, thrombolytics, antiplatelet medicines, and other drugs can be used to stabilise the heart, break up clots, and stop additional damage.
- Defibrillation and CPR: In situations of cardiac arrest, prompt defibrillation and CPR are essential for survival.
- Angioplasty & Stenting: To clear clogged arteries and replenish the heart's blood supply, angioplasty and stenting are frequently carried out during or right after a heart attack.
- Coronary Artery Bypass Surgery: Bypass surgery may be required to restore sufficient blood flow to the heart muscle in situations where numerous coronary arteries are blocked.
- Implanted Technology: Implanted devices that control heart rhythm and avert sudden cardiac death include pacemakers, implanted cardioverter-defibrillators (ICDs), and other devices.
- Emergency Surgery: To repair damage from an aortic dissection or other potentially fatal diseases, emergency surgery may be necessary in certain situations.
What Are the Prevention Tips for Cardiac Emergencies?
Prevention of cardiac emergencies involves managing risk factors and making healthy lifestyle choices, such as:
- Avoid unhealthy eating by removing food items like bacon, processed snacks, fast food, red meat, sugar drinks, and popcorns.
- Physical activity strengthens the heart and improves circulation.
- Quitting smoking to reduce the risk of cardiac emergencies.
- Managing chronic stress.
- Control Blood Pressure and Cholesterol
- Routine medical cardiac check-ups
- Medication Adherence.
Conclusion
Cardiac emergencies are dangerous and fatal situations that need to be treated right away. Your chance of having a cardiac emergency can be considerably decreased by being informed of the risks and implementing preventive actions. You must realise that timely treatment and early discovery can prevent fatalities. Therefore, for quicker action and better results, speak with your health expert and comprehend the symptoms, causes, and available treatments.
FAQs
How to handle cardiac emergencies?
To save lives, handling cardiac crises demands prompt and immediate response. This is how you reply:
- Call Emergency Services: If you need expert assistance right away, call emergency services.
- Perform CPR: If the victim is not breathing or responding, begin CPR.
- Apply an AED: If it is accessible, use an automated external defibrillator (AED).
- Maintain the Person's Calm: As help arrives, assist the patient in maintaining composure and comfort.
.webp&w=3840&q=75)