Endoscopic Retrograde Cholangio-Pancreatography or more popularly known as ERCP is a medical procedure used to diagnose and treat conditions of the liver, gallbladder, bile ducts and pancreas.
Endoscopic Retrograde Cholangiopancreatography or more popularly known as ERCP is a medical procedure used to diagnose and treat conditions of the liver, gallbladder, bile ducts, and pancreas. This method uses a combination of endoscopy and fluoroscopy to assess the organs in detail and check for any problems. Moreover, in some cases, ERCP can also be used to treat problems in these parts of the digestive system.
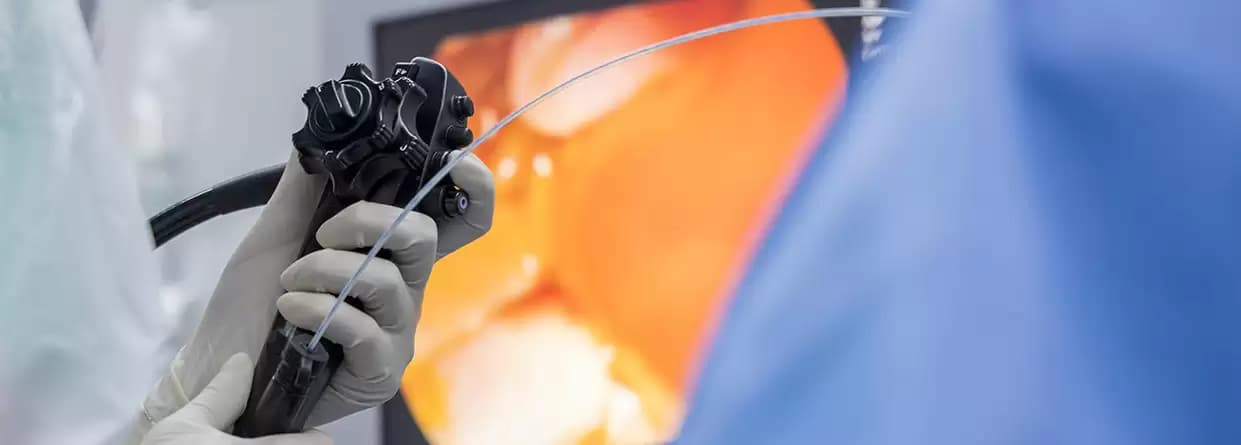
In an ERCP method, an endoscope – a thin, lighted, flexible tube – is placed in the mouth and passed to the stomach and the upper part of the small intestine. In the small intestine, a small plastic tube flows through the endoscope into a tiny opening in the small intestine. Post this, a dye is injected and X-Rays are taken to assess existing or potential problem areas. The method can also be used to further diagnose any abnormal results received from a blood test, ultrasound or CT scan. The most common reasons, why a person is asked to undertake an ERCP examination, include symptoms such as pain in the abdomen, unexplained weight loss, jaundice, stones or abnormal mass in the concerned organs.
Moreover, an ERCP can also be used in gallbladder surgery or to remove stones of the bile duct. Complications from gallbladder surgery can be diagnosed and treated with ERCP in some cases. The method is also useful to diagnose any type of cancer, as well as any non-cancerous tumors. Also, for patients suffering from pancreatic disease, ERCP can be used to study the conditions, determine the need for surgery, as well the best surgical method for treatment.
A patient is advised to undertake an ERCP procedure to diagnose unexplained abdominal pain or jaundice. Moreover, it is also useful in cases of liver cancer, pancreatitis, or any other problem related to the pancreas or bile duct. Some other cases where an ERCP might be recommended include, but are not limited to:
Before the procedure, the patient would be required to be empty stomach and not drink or eat anything at least for 8 hours prior to the procedure. Also, current medications will be adjusted and eliminated depending on case to case. Moreover, any chronic health problems must be in the knowledge of the doctor. Once cleared, the patient will be sedated to begin the procedure.
During the procedure, the gastroenterologist (a doctor who specializes in gastrointestinal problems) uses an endoscope – a thin, light, flexible tube mounted with a camera and light – to study the inside of the patient’s digestive system. Once placed, the doctor then spots the point where the bile duct enters the intestine and then places a tiny tube (catheter) into the targeted duct, and injects contrasting material to take images of the internal functioning and condition of the organs. The contrasting agent – mostly a dye – enables the doctor to examine the bile ducts, gallbladder, and pancreatic ducts through X-Rays. This helps in identifying the source of an existing problem or risks of a potential problem, which then can be treated using the following medical procedures:
Sphincterotomy: This method involves making a microscopic incision in the pancreatic duct or the bile duct, enabling the pancreatic juice, bile, and small gallstones to drain completely.
Stent Placement: An ERCP can also help in drainage by placing a stent – a drainage tube – in the bile duct or the pancreatic duct, to keep it open.
Gallstone Removal: With the help of ERCP it is possible to remove gallstones from the bile duct.
Post the procedure, the patient is taken to the recovery room and observed till the blood pressure, pulse, and breathing stabilizes. The patient is discharged as soon as these parameters stabilize and there is no risk of potential complications. However, the patient does not have to drink or eat anything till the time the gag reflex has returned. After the procedure, the patient might experience, a sore throat and pain in swallowing for some days.
That said, the patient can return to normal activities the next day of the procedure. In case, the patient experiences fever redness, swelling, abdominal pain, blood stool, throat or chest pain, or any other serious after-effects – medical attention must be sought immediately.
An ERCP is considered a relatively safe and low-risk procedure. However, there may be a chance of some complications arising, such as:
In all, an ERCP is a safe and very useful procedure that provides effective results in no time and has a shorter hospital stay, as well as a faster recovery period.
Written and Verified by:
.webp&w=256&q=75)
Dr. Anil Kumar Jangid is a Senior Consultant in Gastroenterology Dept. at CK Birla Hospital, Jaipur with over 13 years of experience. He specializes in treating acidity, abdominal pain, jaundice, and ulcers.
Similar Gastro Science Blogs
Book Your Appointment TODAY
© 2024 RBH Jaipur. All Rights Reserved.